Souci Louis, VMD1,2; Miguella Mark-Carew, PhD2; Matthew Biggerstaff, ScD3; Jonathan Yoder, MPH2; Alexandria B. Boehm, PhD4; Marlene Ok. Wolfe, PhD5; Matthew Flood, PhD6; Susan Peters, DVM6; Mary Grace Stobierski, DVM6; Joseph Coyle, MPH6; Matthew T. Leslie, DVM, PhD7; Mallory Sinner, MPH7; Crack of dawn Nims, MPH7; Victoria Salinas, MPH8; Layla Lustri, MPH8; Heidi Bojes, PhD8; Varun Shetty, MD8; Elisabeth Burnor, MSc9; Angela Rabe, MAS9; Guinevere Ellison-Giles, MPH9; Alexander T. Yu, MD9; Austin Bell, MPH10; Stephanie Meyer, MPH10; Ruth Lynfield, MD10; Melissa Sutton, MD11; Ryan Scholz, DVM12; Rebecca Falender, DVM13; Shannon Matzinger, PhD14; Allison Wheeler, MSPH14; Farah S. Ahmed, PhD15; John Anderson, PhD15; Kate Harris, MS16; Austin Walkins, MS16; Surabhi Bohra, MHS17; Victoria O’Dell, MPH17; Virginia T. Guidry, PhD18; Ariel Christensen, MPH18; Zack Moore, MD18; Erica Wilson, MD18; Joshua L. Clayton, PhD19; Hannah Parsons, MPH19; Krista Kniss, MPH3; Alicia Budd, MPH3; Jeffrey W. Mercante, PhD2; Heather E. Reese, PhD2; Michael Welton, PhD20; Megan Bias, MPH2; Jenna Webb, MPH21; Daniel Cornforth, PhD2; Scott Santibañez, MD, DMin2; Rieza H. Soelaeman, PhD2; Manpreet Kaur, MPH2; Amy E. Kirby, PhD2; John R. Barnes, PhD2; Nicole Fehrenbach, MPP2; Sonja J. Olsen, PhD3; Margaret A. Honein, PhD2 (View creator affiliations)
View instructed citationSummary
What’s already identified about this subject?
Wastewater surveillance can come across influenza An epidemic and the H5 subtype, despite the fact that present checking out does no longer distinguish between human and animal assets.
What’s added through this record?
Throughout Would possibly 12–July 13, 2024, prime influenza An epidemic ranges had been detected in wastewater in 4 states, together with 3 states with seasonal human influenza virus job famous all over this time. The H5 subtype used to be detected in wastewater in 9 states; follow-up investigations in lots of of those states printed most probably animal-related assets, together with the ones linked to take advantage of processing.
What are the consequences for public well being observe?
Early paintings to interpret influenza An epidemic and H5 subtype detections in wastewater can assist with public well being preparedness and reaction for the impending breathing sickness season.
Summary
As a part of the reaction to the extremely pathogenic avian influenza A(H5N1) virus outbreak in U.S. livestock and poultry and the related human circumstances, CDC and companions are tracking influenza An epidemic ranges and detection of the H5 subtype in wastewater. Amongst 48 states and the District of Columbia that carried out influenza A checking out of wastewater all over Would possibly 12–July 13, 2024, a weekly moderate of 309 websites in 38 states had enough knowledge for evaluation, and 11 websites in 4 states reported prime ranges of influenza An epidemic. H5 subtype checking out used to be carried out at 203 websites in 41 states, with H5 detections at 24 websites in 9 states. For every detection or prime degree, CDC and state and native well being departments evaluated knowledge from different influenza surveillance methods and partnered with wastewater utilities and agriculture departments to analyze attainable assets. A few of the 4 states with prime influenza An epidemic ranges detected in wastewater, 3 states had corresponding proof of human influenza job from different influenza surveillance methods. A few of the 24 websites with H5 detections, 15 known animal assets inside the sewershed or adjoining county, together with 8 milk-processing inputs. Knowledge from those early investigations can assist well being officers optimize using wastewater surveillance all over the impending breathing sickness season.
Advent
Wastewater surveillance is used to observe human losing of pathogens, together with SARS-CoV-2, at a neighborhood degree and is unbiased of signs, checking out get entry to, and care-seeking conduct (1). Some websites have carried out wastewater influenza virus surveillance for a number of years, and findings have correlated with conventional influenza surveillance measures (2–6). The zoonotic outbreak of extremely pathogenic avian influenza (HPAI) A(H5N1) in america has ended in 13 showed human circumstances all over January–August 2024.* As a part of the reaction to this outbreak, CDC and state and native well being departments are the use of wastewater surveillance to observe influenza An epidemic and the H5 subtype; alternatively, present checking out ways can not distinguish between human and animal assets. This record summarizes knowledge from the primary 9 weeks of tracking influenza An epidemic and the H5 subtype in wastewater throughout america, together with findings from collaborations with state and native well being departments to analyze attainable assets all over the continuing H5N1 public well being reaction.
Strategies
Influenza A Virus Trying out
Wastewater samples accrued from roughly 750 websites in 48 states and the District of Columbia all over Would possibly 12–July 13, 2024, had been examined for influenza An epidemic through state and native well being departments, a CDC contractor, or an educational spouse program (WastewaterSCAN [ and results were submitted to CDC’s Data Collation and Integration for Public Health Event Response (DECIPHER) pipeline.† Although not specific to the H5N1 subtype, the influenza A virus testing performed routinely by partners across the United States frequently detects any influenza A virus, including seasonal and H5 subtypes. For this analysis, concentrations of influenza A virus in wastewater were measured using digital polymerase chain reaction testing with various primer and probe oligonucleotides and assay conditions that were optimized by each laboratory (7). For each site, the percentile of the most recent week’s normalized concentration was calculated compared with the normalized concentrations reported during October 1, 2023–March 2, 2024, corresponding to the portion of the influenza season before the reported HPAI A(H5N1) outbreak in dairy cattle. Influenza A virus levels at each site were categorized as high, above average, moderate, low, or minimal.§
Influenza A(H5) Virus Subtype Testing
In April 2024, a digital polymerase chain reaction assay for the H5 hemagglutinin gene of the influenza A virus was developed and evaluated by WastewaterSCAN for testing wastewater and detected H5 viral RNA in wastewater samples from multiple locations experiencing cattle outbreaks (7). In May 2024, routine H5 testing was implemented at 193 sites (reduced to 152 sites by July 1, 2024) across 41 states, and results were displayed on a public dashboard¶; H5 testing was also implemented at 10 additional sites in one state, for a total of 203 sites with any H5 testing. CDC’s wastewater DECIPHER data pipeline was updated to receive influenza A virus subtyping results, and submission of H5 virus data commenced in July 2024.
Collaboration To Evaluate Wastewater Signals
CDC notified jurisdictions of high influenza A virus levels on a weekly basis; notification of new H5 detections were provided daily. CDC provided jurisdictions with a checklist** for follow-up, which included reviewing human influenza surveillance systems and characterizing sewershed inputs (substances that flow into sewer pipes) in partnership with wastewater utilities, departments of agriculture, and others. This activity was reviewed by CDC, deemed not research, and was conducted consistent with applicable federal law and CDC policy.††
Results
Detection of High Influenza A Virus Levels
Among an average of 309 wastewater sites with sufficient data for analysis for ≥1 week during May 12–July 13 (Figure), 11 sites in four states (California, Illinois, Kansas, and Oregon) had high influenza A levels detected at least once (Table). In three of these states, six wastewater sites with high influenza A virus levels were in communities with evidence of human influenza activity, based on other surveillance. The influenza A virus wastewater data are not specific to H5, and none of these four states reported H5 human influenza cases, nor did they report any confirmed cases in livestock herds or poultry within their sewersheds or counties during this time.§§ Most of these sites reported open or combined sewersheds, and some sites identified specific potential sources of animal input.¶¶
H5 Subtype Detections
Among 41 states with influenza A H5 testing in wastewater, nine states (California, Colorado, Idaho, Iowa, Michigan, Minnesota, North Carolina, South Dakota, and Texas) reported one or more H5 detections during May 12–July 13, and 32 states did not have H5 detections during this period. The nine states with H5 detections in wastewater included seven states with an HPAI A(H5N1)–infected herd reported during this period and one additional state with an infected herd reported before this period. Two of these nine states (Colorado and Michigan) reported confirmed human cases of HPAI A(H5N1) virus infection during this time.*** Among the 32 states with H5 testing in wastewater and no H5 detections in wastewater during the analysis period, 30 (94%) had no herds with HPAI A(H5N1) virus infections reported during this time, and two had infected herds reported only before this period.
In determining inputs to specific wastewater sites, 15 of 24 sites (63%) with H5 detections identified some animal inputs within the sewershed or county. Eight of 24 sites (33%) identified milk-processing inputs within the sewershed catchment area. Additional inputs noted were meat processing, dairy operations within the sewershed or adjacent county, other sources of livestock waste (e.g., truck wash), wild bird inputs, and domestic poultry farms within the sewershed or county.†††
Discussion
During May 12–July 13, most U.S. wastewater sites tested did not have high influenza A virus levels or any detections of the H5 subtype. Among the sites that did have high influenza A virus levels, the most frequent finding was corresponding evidence of human influenza A virus activity in the community. Among sites that reported H5 detections in wastewater, all but one were in a state with reported infected dairy herds during or before the surveillance period, and animal-related inputs such as effluent from milk-processing plants and suspected contributions from wild birds were frequently reported. These differences highlight the importance of influenza A virus subtyping to provide data specific to HPAI outbreaks.
The findings in this report underscore the importance of using a One Health approach that leverages multisectoral collaboration to understand the complexity of inputs from animal and human sources.§§§ The current zoonotic outbreak of HPAI A(H5N1) virus highlights the importance of coordination across health, agriculture, wildlife, food safety, and other partners. Investigations into wastewater signals also require coordination among public health, academic, municipal water treatment, and community partners. Influenza A(H5N1) virus has been found at very high concentrations in milk from infected cows (8); investigations of influenza A and H5 virus signals in wastewater suggest that milk effluent from milk-processing facilities can be a major contributor to H5 viral particles in wastewater (7,9). Monitoring influenza A viruses and specific influenza A virus subtypes in wastewater might serve as One Health surveillance indicators of the presence of influenza viruses in a community. Further, existing human clinical influenza surveillance systems are essential for quickly identifying H5 virus infections in humans and monitoring seasonal influenza virus activity.
Public health agencies that conduct wastewater monitoring to complement influenza surveillance systems should be prepared to add influenza A virus subtype testing when needed to improve understanding of influenza A virus detections in the context of the current HPAI A(H5N1) outbreak. CDC-funded National Wastewater Surveillance System’s Centers of Excellence are expanding influenza A virus testing and subtyping, which can contribute to source investigations and be deployed at strategic times and places.¶¶¶ Although this report focused on comparing influenza A virus levels with those from the previous season and identifying H5 detections, subtyping for seasonal influenza A(H1) and A(H3) viruses in wastewater samples and using state and national viral activity levels to monitor influenza A across sites can help with interpretation of wastewater surveillance data during the upcoming influenza season.****
A critical need for clear communication about the meaning of detection of influenza A virus and subtypes exists. Data dashboards can provide regular wastewater surveillance updates to the public, the media, and health care providers; however, these data need to be accompanied by clear public health interpretations focusing on potential human risk and public health actions, which could include alerts to health care providers or increasing availability of testing or vaccines as has been done for SARS-CoV-2 and mpox. Activities to monitor influenza A virus and subtypes using wastewater data are likely to evolve as the methodologies and interpretation are further evaluated and refined.
Limitations
The findings in this report are subject to at least five limitations. First, although influenza viruses can be detected in wastewater, current techniques cannot distinguish between human and animal sources, and the current approach for H5 testing in wastewater is not specific to HPAI A(H5N1) viruses; H5 detections in wastewater might reflect animal rather than human infections and might be detection of low pathogenic avian influenza rather than HPAI A(H5N1) viruses. Second, limited data are available regarding the proportion of persons infected with influenza viruses who shed virus in urine or feces, and how the concentration of viral shedding varies by subtype and across the course of illness (10). Third, population wastewater surveillance coverage varies substantially by state; therefore, data are most informative when used in conjunction with clinical human influenza surveillance data. Fourth, states reported information on the investigations of sewershed inputs for sites with high influenza A virus levels or H5 detections, but comparison information for sites without these signals was not collected; therefore, epidemiologic measures for these possible associations could not be generated. Finally, the comprehensiveness of data collection after a signal in wastewater varied widely. Public health investigations into potential sources of H5 viruses in wastewater can be complex (e.g., milk-processing inputs can include milk from other states) and might support or refute likely sources of H5 without providing definitive conclusions.
Implications for Public Health Practice
Lessons learned during early follow-up investigations of wastewater signals can help health officials implement an improved measure of influenza A virus levels in wastewater and optimize the use of wastewater surveillance during the upcoming respiratory illness season. The findings in this report, and data from wastewater surveillance in general, can complement traditional influenza surveillance systems. A One Health approach with multisectoral collaboration and data-informed guidance on when and how to use influenza virus subtyping of wastewater might enhance the public health response to the current outbreak.
Acknowledgments
Rachel Herlihy, Colorado Department of Public Health & Environment; Thomas Clerkin, Rachel Noble, University of North Carolina at Chapel Hill; James Wendt, Charles Williams, Illinois Department of Public Health; Elizabeth Coke, Libby Horter, Amanda Raziano, Jessica Ricaldi, Diana Valencia, National Center for Emerging and Zoonotic Infectious Diseases, CDC; Peter Daly, Shunte Moon, National Center for Immunization and Respiratory Diseases, CDC; Elizabeth Daly, Marci Layton, Lindsay Pierce, Council of State and Territorial Epidemiologists; Water Environment Federation.
1Epidemic Intelligence Service, CDC; 2Division of Infectious Disease Readiness and Innovation, National Center for Emerging and Zoonotic Infectious Diseases, CDC; 3Influenza Division, National Center for Immunization and Respiratory Diseases, CDC; 4Department of Civil & Environmental Engineering, School of Engineering and Doerr School of Sustainability, Stanford University, Stanford, California; 5Gangarosa Department of Environmental Health, Rollins School of Public Health, Emory University, Atlanta, Georgia; 6Michigan Department of Health and Human Services; 7Illinois Department of Public Health; 8Texas Department of State Health Services; 9Center for Infectious Diseases, Division of Communicable Disease Control, California Department of Public Health, Richmond, California; 10Minnesota Department of Health; 11Public Health Division, Oregon Health Authority, Portland, Oregon; 12Oregon Department of Agriculture; 13Oregon State University; Corvallis, Oregon; 14Colorado Department of Public Health & Environment; 15Kansas Department of Health and Environment; 16City of Boise, Boise, Idaho; 17Central District Health; 18North Carolina Department of Health and Human Services; 19South Dakota Department of Health; 20Global Government Solutions Corporation, San Antonio, Texas; 21Chenega Corporation, Atlanta, Georgia.
References
Kilaru P, Hill D, Anderson K, et al. Wastewater surveillance for infectious disease: a systematic review. Am J Epidemiol 2023;192:305–22. PMID:36227259
Faherty EAG, Yuce D, Korban C, et al. Correlation of wastewater surveillance data with traditional influenza surveillance measures in Cook County, Illinois, October 2022–April 2023. Sci Total Environ 2024;912:169551. PMID:38135071
Schoen ME, Bidwell AL, Wolfe MK, Boehm AB. United States influenza 2022–2023 season characteristics as inferred from wastewater solids, influenza hospitalization, and syndromic data. Environ Sci Technol 2023;57:20542–50. PMID:38014848
DeJonge PM, Adams C, Pray I, et al. Wastewater surveillance data as a complement to emergency department visit data for tracking incidence of influenza A and respiratory syncytial virus—Wisconsin, August 2022–March 2023. MMWR Morb Mortal Wkly Rep 2023;72:1005–9. PMID:37708080
Boehm AB, Hughes B, Duong D, et al. Wastewater concentrations of human influenza, metapneumovirus, parainfluenza, respiratory syncytial virus, rhinovirus, and seasonal coronavirus nucleic-acids during the COVID-19 pandemic: a surveillance study. Lancet Microbe 2023;4:e340–8. PMID:36965504
Lehto KM, Länsivaara A, Hyder R, et al.; WastPan Study Group. Wastewater-based surveillance is an efficient monitoring tool for tracking influenza A in the community. Water Res 2024;257:121650. PMID:38692254
Wolfe MK, Duong D, Shelden B, et al. Detection of hemagglutinin H5 influenza A virus sequence in municipal wastewater solids at wastewater treatment plants with increases in influenza A in spring, 2024. Environ Sci Technol Lett 2024;11:526–32.
Caserta LC, Frye EA, Butt SL, et al. From birds to mammals: spillover of highly pathogenic avian influenza H5N1 virus to dairy cattle led to efficient intra- and interspecies transmission. bioRxiv [Preprint posted online May 22, 2024].
Le Sage V, Campbell AJ, Reed DS, Duprex WP, Lakdawala SS. Endurance of influenza H5N1 and H1N1 viruses in unpasteurized milk on milking unit surfaces. Emerg Infect Dis 2024;30:1721–3. PMID:38914418
Lowry SA, Wolfe MK, Boehm AB. Respiration virus concentrations in human excretions that give a contribution to wastewater: a scientific overview and meta-analysis. J Water Well being 2023;21:831–48. PMID:37387346
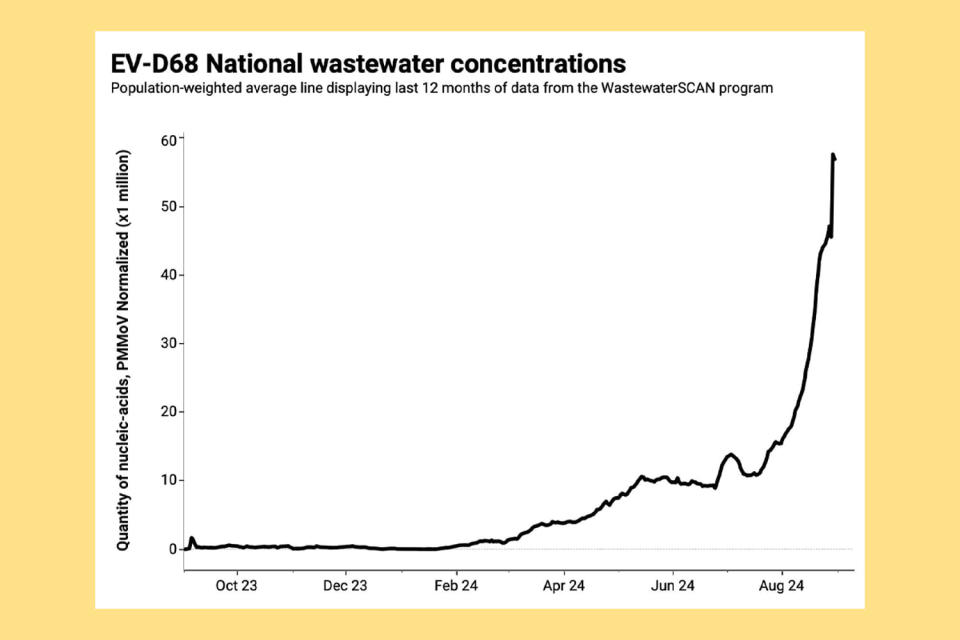
![]() FIGURE. Influenza An epidemic and H5 subtype checking out in wastewater and websites with prime ranges* of influenza An epidemic or H5 detections reported to CDC — United States, Would possibly 12–July 13, 2024†
FIGURE. Influenza An epidemic and H5 subtype checking out in wastewater and websites with prime ranges* of influenza An epidemic or H5 detections reported to CDC — United States, Would possibly 12–July 13, 2024†

Abbreviation: DC = District of Columbia.
* Influenza A ranges had been classified as being at a prime (≥eightieth percentile when put next with earlier influenza season), above moderate (sixtieth to <eightieth percentile), average (fortieth to <sixtieth percentile), low (twentieth to <fortieth percentile), or minimum (<twentieth percentile) degree, or as having inadequate knowledge for evaluation.
† Websites with enough knowledge for evaluation integrated those who had influenza A wastewater checking out knowledge sooner than October 1, 2023, had 10 or extra samples through which influenza A used to be detected all over October 1, 2023–March 2, 2024, had six or extra samples examined all over October 1, 2023–January 1, 2024, and submitted knowledge within the 2 weeks sooner than evaluation.
TABLE. Traits of websites with prime* influenza An epidemic job or H5 detection in wastewater — United States, Would possibly 12–July 13, 2024![]()
Feature
No. (%)
Influenza An epidemic checking out†
H5 subtype checking out§
States with prime degree¶
n = 4
Websites with prime degree
n = 11
States with H5 detections**
n = 9
Websites with H5 detections
n = 24
Human influenza surveillance alerts
Proof of human influenza job according to different surveillance methods
3 (75)
6 (54)
1 (11)
3 (13)
Form of sewershed
Mixed (open)
NA
8 (73)
NA
5 (21)
Separate (closed)
NA
3 (27)
NA
17 (71)
Data no longer equipped
NA
0 (—)
NA
2 (8)
Attainable sign supply (inside of sewershed or county)††
Dairy or cattle
Dairy operations
0 (—)
0 (—)
3 (33)
5 (21)
Farm animals truck wash
2 (50)
2 (18)
1 (11)
3 (13)
Milk processing
3 (75)
3 (27)
4 (44)
8 (33)
Meat processing
0 (—)
0 (—)
5 (56)
7 (29)
No dairy or cattle inputs known
4 (100)
5 (45)
4 (44)
10 (42)
Data no longer equipped
1 (9)
1 (9)
1 (11)
2 (8)
Avian
Wild hen inputs suspected as conceivable
2 (50)
6 (55)
4 (44)
10 (42)
Lively poultry circumstances
0 (—)
0 (—)
2 (22)
2 (8)
No avian inputs known
2 (50)
4 (36)
6 (67)
11 (46)
Data no longer equipped
1 (9)
1 (9)
1 (11)
2 (8)
Any dairy, cattle, or avian enter
3 (75)
8 (73)
8 (89)
15 (63)
Data no longer equipped
1 (9)
1 (9)
1 (11)
2 (8)
Different
Recognized human influenza H5 circumstances all over this era
0 (—)
NA
2 (22)§§
NA
H5 showed circumstances in cattle herds all over this era
0 (—)
NA
7 (78)¶¶
NA
Abbreviation: NA = no longer acceptable.
* Influenza A ranges had been classified as being at a prime (≥eightieth percentile when put next with earlier influenza season), above moderate (sixtieth to <eightieth percentile), average (fortieth to <sixtieth percentile), low (twentieth to <fortieth percentile), or minimum (<twentieth percentile) degree, or as having inadequate knowledge for evaluation.
† At a mean of 309 weekly websites in 38 states with enough knowledge for evaluation.
§ At 203 websites in 41 states.
¶ The next jurisdictions had a number of websites with a prime influenza A degree all over the 9-week length: California, Illinois, Kansas, and Oregon.
** The next jurisdictions had a number of websites with an H5 detection all over the 9-week length: California, Colorado, Idaho, Iowa, Michigan, Minnesota, North Carolina, South Dakota, and Texas.
†† Every website had the choice to choose a couple of attainable assets; thus, those classes and responses inside of classes don’t seem to be mutually unique.
§§ Colorado and Michigan had known human circumstances of influenza A(H5N1) virus an infection all over this era.
¶¶ Colorado, Idaho, Iowa, Michigan, Minnesota, South Dakota, and Texas had publicly reported influenza A(H5N1) virus infections in dairy livestock herds all over this era.
Steered quotation for this text: Louis S, Mark-Carew M, Biggerstaff M, et al. Wastewater Surveillance for Influenza A Virus and H5 Subtype Concurrent with the Extremely Pathogenic Avian Influenza A(H5N1) Virus Outbreak in Livestock and Poultry and Related Human Instances — United States, Would possibly 12–July 13, 2024. MMWR Morb Mortal Wkly Rep 2024;73:804–809. DOI:
MMWR and Morbidity and Mortality Weekly File are provider marks of the U.S. Division of Well being and Human Products and services.
Use of business names and industrial assets is for identity most effective and does no longer suggest endorsement through the U.S. Division of
Well being and Human Products and services.
References to non-CDC websites at the Web are
equipped as a provider to MMWR readers and don’t represent or suggest
endorsement of those organizations or their techniques through CDC or the U.S.
Division of Well being and Human Products and services. CDC isn’t chargeable for the content material
of pages discovered at those websites. URL addresses indexed in MMWR had been present as of
the date of newsletter.
All HTML variations of MMWR articles are generated from ultimate proofs thru an automatic procedure.
This conversion would possibly lead to persona translation or layout mistakes within the HTML model.
Customers are referred to the digital PDF model (
and/or the unique MMWR paper replica for printable variations of professional textual content, figures, and tables.
Questions or messages relating to mistakes in formatting must be addressed to
mmwrq@cdc.gov.