November 18, 2024 Through: Karen Peralta Martinez
New analysis from the College of Pittsburgh uncovers how inhaled area mud mites, a not unusual cause of allergic bronchial asthma, turn on the immune machine and pressure this illness in mice.
The findings, printed lately in Nature Immunology, be offering necessary insights into how apparently risk free components comparable to mud mites, puppy dander and pollen can conquer the immune machine to cause hypersensitive reactions and may ultimately pave the way in which for figuring out new therapeutics to regard and set up allergic bronchial asthma.

 Dr. Amanda C. Poholek
Dr. Amanda C. Poholek
“We continuously call to mind the immune machine as a military that fights the dangerous guys,” stated senior creator Dr. Amanda C. Poholek, director of the Well being Sciences Sequencing Core and assistant professor within the Division of Immunology at Pitt’s Faculty of Medication. “And whilst that’s true, as a rule your immune machine isn’t encountering pathogens however coping with mud and pollen that you just breathe in, crops and animals that you just devour, and issues that you just contact within the setting. A large query that motivates my analysis is: How does our immune machine know to answer pathogens and to not self and the surroundings?”
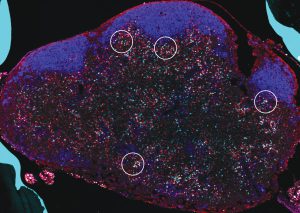
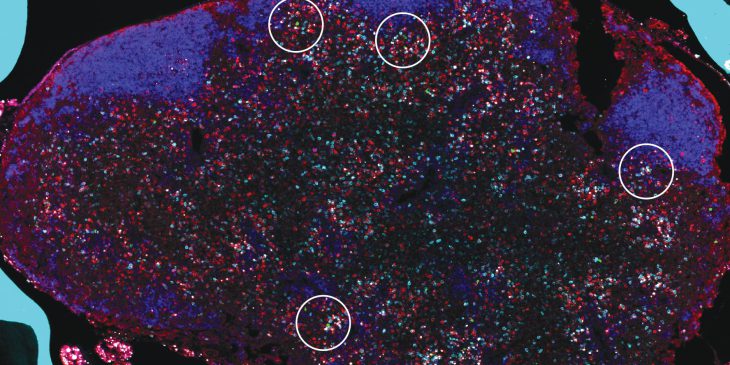
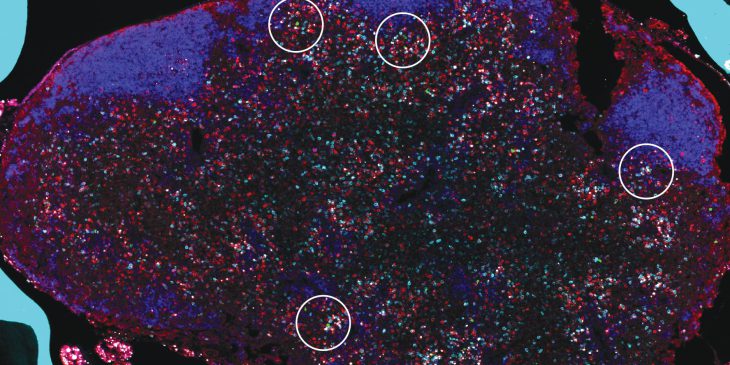
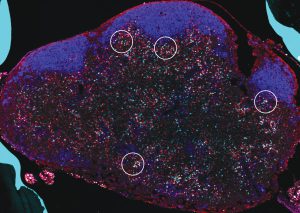 Mouse lymph node with hotspots of IL2 job rotated (CREDIT: Kun He)
Mouse lymph node with hotspots of IL2 job rotated (CREDIT: Kun He)
When the immune machine does this task accurately, it’s referred to as immune tolerance. But if tolerance breaks down, normally risk free environmental allergens can turn on T Helper 2 (Th2) cells, which might be a kind of immune mobile that drives irritation in allergic bronchial asthma and different allergic illnesses.
Allergic bronchial asthma is the commonest type of bronchial asthma, characterised by means of signs comparable to coughing, chest tightness, shortness of breath and wheezing. This debilitating situation is on the upward thrust international and puts a considerable burden at the well being care machine, in line with Poholek.
To be informed extra about how allergens turn on Th2 cells and purpose allergic bronchial asthma, Poholek and her staff used a mouse type of the illness precipitated by means of inhalation of area mud mites. This type is a extra correct illustration of ways people come across allergens in comparison to research that used under-the-skin or systemic injections of allergen.
The usage of new gear that allowed them to trace Th2 cells and notice precisely after they get activated and the place they went, the researchers discovered that in accordance with inhaled area mud mite, a particular molecular pathway involving a protein known as BLIMP1 was once had to generate Th2 cells within the lymph node. Those cells then transfer to the lung and pressure illness. By contrast, when area mud mite is injected, that molecular pathway isn’t wanted.
Additionally they discovered that two signaling molecules, or cytokines, known as IL2 and IL10 have been required for expression of BLIMP1.
“IL10 is in most cases considered an anti inflammatory cytokine, which dampens immune responses, so we have been truly shocked to seek out that it was once if truth be told selling irritation,” stated Poholek. “This discovering opens that door to healing choices focused on IL10, which hadn’t prior to now been regarded as, in particular for newly recognized sufferers.”
In step with Poholek, maximum sufferers with allergic bronchial asthma obtain steroids, which deal with the indications however now not the foundation of the illness. There’s a massive want for brand spanking new remedies that let early intervention earlier than allergic bronchial asthma reasons long-term harm to the airlines.
When the researchers mapped the positioning of Th2 activation within the lymph node, they have been additionally shocked to seek out hotspots of IL2 job.
“IL2 is an overly distinguished cytokine, so we anticipated that it will be dispersed right through the lymph node,” stated Poholek. “As a substitute, we found out that IL2 was once localized to positive areas. Now, now we have much more paintings to determine how those areas shape and whether or not disrupting those areas may disrupt the formation of Th2 cells, halting allergic bronchial asthma.”
In collaboration with colleagues within the Pitt Department of Pulmonology, Allergic reaction, Crucial Care and Sleep Medication, Poholek may be making plans to take a look at lung tissue samples to research whether or not IL2 and IL10 may be necessary drivers of Th2 cells in sufferers with allergic bronchial asthma and discover doable avenues for creating new healing choices.
Karen Peralta Martinez is a Ph.D. candidate within the College of Pittsburgh Division of Organic Sciences. She is taking part within the UPMC Science Writing Mentorship Program.
Percentage this on:![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]() Copied!
Copied!