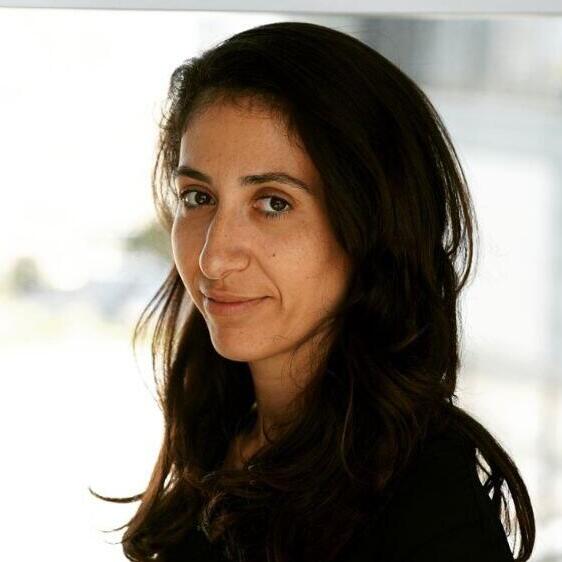
Blue Cross Blue Shield of Massachusetts is postponing a contentious change in insurance coverage for endoscopic procedures that was set to take effect on January 1. This change was prompted by the report in the Telegram & Gazette revealing the plan to cover full sedation for procedures such as colonoscopy only if it was deemed medically necessary by a doctor. Without this determination, the insurance would only cover moderate sedation. This change was opposed by some healthcare providers and doctors, who argued that it could limit access to colonoscopies and compromise patient safety. Others claimed that the motive behind the change was to reduce costs, as full sedation is more expensive compared to moderate sedation. Blue Cross attributed the delay to the confusion about the policy. Dr. Sandhya Rao, chief medical officer and senior vice president at Blue Cross Blue Shield of Massachusetts, stated that the confusion stemmed from inaccurate information about the coverage for different types of sedation for these procedures. As a result of this confusion, the enforcement of this policy has been paused, while efforts are made to ensure that members understand all their options for colon cancer screening and sedation and are confident that they are receiving the best care for them.  Rao indicated in the T&G story that Blue Cross altered the policy to align with updated guidelines from the American Society of Gastrointestinal Endoscopy due to health risks associated with full sedation. In following these guidelines, the insurer aims to provide its members with access to high-quality, safe, and affordable care. Blue Cross processes claims for about 74,000 colonoscopy patients yearly in Massachusetts, with the majority being done under full sedation. A colonoscopy screens for colorectal cancer, the second-leading cause of cancer-related deaths in the U.S., according to the American Cancer Society. Contact Henry Schwan at henry.schwan@telegram.com. Follow him on X: @henrytelegram.
Rao indicated in the T&G story that Blue Cross altered the policy to align with updated guidelines from the American Society of Gastrointestinal Endoscopy due to health risks associated with full sedation. In following these guidelines, the insurer aims to provide its members with access to high-quality, safe, and affordable care. Blue Cross processes claims for about 74,000 colonoscopy patients yearly in Massachusetts, with the majority being done under full sedation. A colonoscopy screens for colorectal cancer, the second-leading cause of cancer-related deaths in the U.S., according to the American Cancer Society. Contact Henry Schwan at henry.schwan@telegram.com. Follow him on X: @henrytelegram.
Blue Cross Blue Shield of Mass. postpones alteration in colonoscopy coverage